
What Causes UTIs?
Urinary Tract Infections, UTIs, are infections in the bladder and urinary system. There are various risk factors of UTIs that contribute to the development of infections, and it's important to know why they happen and how to stop them.
UTI Causing Bacteria
There are many pathogens, bacteria and fungus, that can cause UTIs as well as UTI like symptoms. Bacteria in our body can also produce antibiotic resistance genes which can make it hard to combat an infection. All these things have markers, DNA, that can found in the urine sample. MyUTI tests for 12 key UTI-causing pathogens as well as the top 3 resistance markers, key indicators of infection. Learn more.
UTIs by Gender
Understanding the causes of Urinary Tract Infections (UTIs) in both women and men is crucial, as it helps in both prevention and effective treatment. The differences in female and male anatomy significantly influence the likelihood and causes of UTIs in each.
UTI Causes in Women
The primary reason for the higher incidence of UTIs in women is the shorter urethra. This shorter passageway makes it easier for bacteria to reach the bladder. During intercourse or day to day activity, normal bacteria from the gut and bowel, like e.coli, can gather in the anal area and then move to the urethra opening which is in close proximity, then make their way up into the bladder.
UTI Causes in Men
While less common, UTIs in men can still pose a significant risk. UTIs in individuals with penises often stem from an enlarged prostate, which can impede urine flow and conditions like prostatitis, or inflammation of the prostate, are linked to an increased risk of UTIs in males. Both an enlarged prostate and inflammation can cause difficulty in fully emptying the bladder which can lead to urine pooling in the urinary tract or bladder, fostering bacterial growth. Uncircumcised men may have a slightly higher risk of UTIs due to bacteria accumulating under the foreskin.
The MyUTI Home Testing Kit
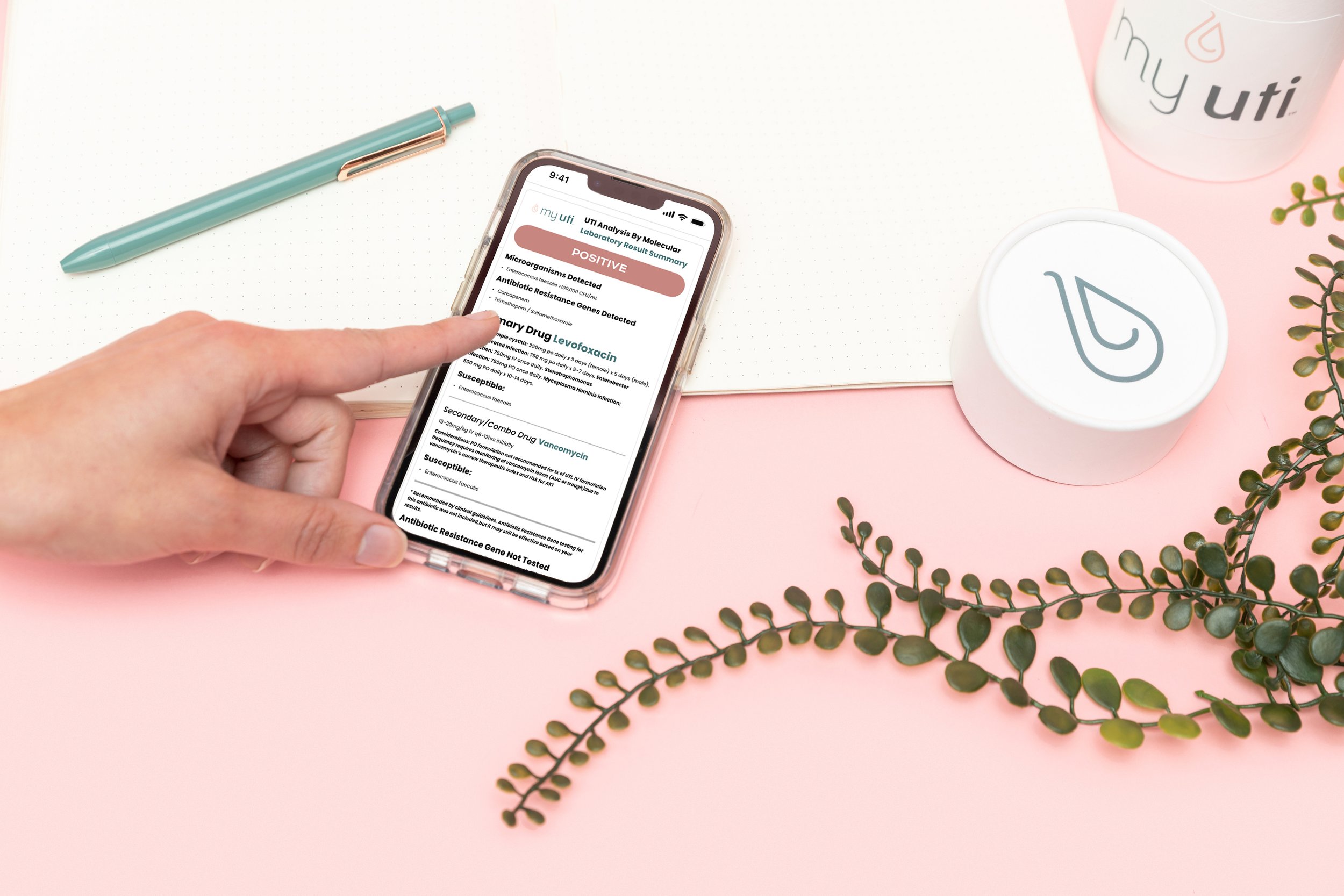
Access to UTI PCR testing on your terms
-
Urine collection cup with easy to follow instructions
PCR testing of top 12 pathogens & 3 antibiotic resistance genes
Personalized lab results
Private portal to monitor testing process
Shipping materials
-
Ground shipping is inlcuded in all orders for free. Upgrade to overnight shipping for additional fee at check-out.
Results provided within 24 hours* from the time the lab receives your sample.
*96% of the time results delivered in 24 hours.
UTIs from Sex
How Germs Move During Sex
When people are sexually active it is not unusual to get a UTI. In the context of sexual activity, it's important to understand how bacteria can be transferred, potentially leading to urinary tract infections (UTIs).
During sex, the close contact and exchange of bodily fluids between partners can facilitate the movement of bacteria. The dynamics of sexual intercourse – the motion and the pressure – can inadvertently push bacteria from the genital or anal areas towards the urethra. This is especially relevant for women, given the anatomical proximity of the urethra to the anus, which shortens the distance bacteria need to travel.This is because germs can move from one person to another and from one area to another. This transfer of bacteria during sexual activity can occur through direct contact via sex or from sex toys.
Adding to this, the use of sex toys can also play a role in this delicate bacterial dance. It’s important to remember the value of keeping these items clean, as they can carry bacteria if not cared for properly. In essence, while sexual activity is a natural and enjoyable part of life, there's also a gentle responsibility to be aware of our health.
UTIs During Pregnancy
When a woman is expecting a baby, her body changes a lot. This can make her more likely to get a UTI. These changes are largely due to hormonal fluctuations and physical changes as the baby grows.
Hormonal Changes and UTI Risk During Pregnancy
During pregnancy, a woman's body experiences significant hormonal changes, notably in levels of estrogen and progesterone. These hormonal shifts can alter the balance of good and bad bacteria in the vagina. Normally, the vaginal flora contains a healthy balance of bacteria, but hormonal changes can disrupt this balance, making it easier for harmful bacteria to proliferate. This imbalance can lead to an increased susceptibility to infections, including UTIs.
Physical Changes and Their Impact
As the baby grows, the uterus expands and starts to exert more pressure on the bladder. This pressure can make it challenging for pregnant women to completely empty their bladder while urinating. A bladder that isn’t fully emptied regularly is more prone to bacterial growth, contributing to the risk of developing UTIs. Moreover, urine during pregnancy may contain higher levels of sugar, providing an ideal breeding ground for bacteria. Additionally, urine during pregnancy may contain elevated sugar levels, which can serve as a breeding ground for bad bacteria to grow.
UTI prevention during pregnancy starts by understanding these hormonal and physical changes, pregnant women can take proactive steps to reduce their risk of UTIs. This includes staying hydrated, using the restroom regularly, managing constipation and seeking regular prenatal care.
UTIs and Menopause
As women enter their 40s homones change again and they begin to go through perimenopause, they may notice being more prone to UTIs and other vaginal infections. Post-menopause, the risk goes up again. This is because of changes in hormones, specifically the decline in estrogen levels, which play a crucial role in maintaining the health of the vaginal and urinary microbiomes.
Hormonal Changes During Perimenopause and Menopause:
Decline in Estrogen: Estrogen plays a vital role in keeping the lining of the bladder and urethra healthy. As women approach menopause, estrogen levels decrease, which can reduce the natural defenses of the urinary tract against bacteria.
Changes in Vaginal Flora: The reduction in estrogen can also alter the vaginal flora. A healthy vagina has a balanced mix of microorganisms, but lower estrogen levels can disrupt this balance, making it easier for harmful bacteria to thrive and potentially cause infections.
Thinning of Urethral and Vaginal Tissues: Lower estrogen levels lead to thinner, less elastic tissues in the vagina and urethra. This physical change can make these areas more susceptible to irritation and infection.
Reduced Lactobacilli: Estrogen helps maintain healthy levels of lactobacilli, a type of bacteria that helps keep the vagina's pH acidic and less hospitable to harmful bacteria. A decline in estrogen means fewer lactobacilli, increasing the risk of UTIs.
Menopause and Urinary Health:
Increased pH Levels: Postmenopause, the vaginal pH becomes less acidic, which can lead to an overgrowth of undesirable bacteria, increasing the risk of UTIs.
Urinary Incontinence: Some women experience urinary incontinence during menopause due to weakened pelvic floor muscles, which can contribute to UTIs.
Navigating UTI prevention during and after menopause can be more intuitive and less of a hassle than it seems. Keeping up with your water intake is essential – it's like giving your urinary tract a regular rinse to keep those pesky bacteria at bay. Combining this with a diet rich in probiotics (think yogurt or kefir) and low in sugar can do wonders for maintaining a healthy bacterial balance in your body. Also, remember to listen to your body's signals; delaying bathroom breaks isn't doing you any favors, so make sure to go when you need to. As for vaginal estrogen therapy, it’s something to consider discussing with your doctor, as it could help in keeping your vaginal health on track.
The Role of Biofilm in UTIs
What Is A Biofilm?
Biofilms are a significant factor in persistent UTI causes and the development of antibiotic-resistant UTIs. They act like protective shields for bacteria, enabling them to adhere to the bladder wall, which can result in recurrent infections. Biofilms are complex, comprising a matrix that guards the bacteria against external threats, including the body's immune response and antibiotic treatments.
Persistent UTIs often recur due to the presence of these biofilms. Bacteria within biofilms can exchange genetic material, including antibiotic resistance genes, making them more formidable against standard treatments. This genetic exchange enhances their survival and complicates treatment efforts, as antibiotics struggle to penetrate the biofilm and fully eradicate the infection.
Addressing biofilms in UTIs involves ongoing research to develop strategies that disrupt biofilm formation or enhance antibiotic effectiveness
How to Treat a Biofilm
Get advanced testing, like MyUTI, to identify the bacteria and resistance genes.
Begin to work with a specialist on a targeted treatment regimen.
Consider supplements that reduce the bacteria's ability to stick to the bladder wall.
Diabetes and UTIs
Why Diabetes Makes UTIs More Likely
People with diabetes are more likely to get UTIs. This is because diabetes can make it hard for the body to fight off germs. High blood sugar can also create the perfect environment for bacteria to grow in the bladder.
Get to the bottom of your UTI symptoms
With the MyUTI Test's advanced PCR technology, you can discover the root cause of your UTI and the effective treatment in just one day.
At home PCR testing with results in a day
Shipped to your doorstep
Easy home collection
Overnight shipment to lab
A targeted treatment plan
Causes Of Frequent UTIs
There are a number of factors that can influence repeat bladder infections. Visit our Learning Center to understand the role bacteria, hormones and antibiotics can play.






Ever wondered about the causes of a bladder biofilm? Learn about the most common pathogens in biofilm and how they work with MyUTI.